Mental Health Month was started in 1949 by the national organization Mental Health America to raise awareness about mental health conditions and the importance of good mental health for everyone. The theme of MHA’s 2022 Mental Health Month Toolkit is “Back to Basics." The goal is to provide foundational knowledge about mental health and mental health conditions. The toolkit also provides information about what people can do if their mental health is a cause for concern. The toolkit is available at mhanational.org/may.
During May, the National Alliance on Mental Illness (NAMI) joins the national movement to raise awareness about mental health. NAMI’s 2022 Mental Health Month theme amplifies the message of “Together for Mental Health." With a growing number of Americans experiencing mental health symptoms, the campaign highlights the importance of joining to together to advocate for improving our nation’s mental healthcare system.
As a provider, you know that creating healthy routines, owning one’s feelings, and connecting with others can positively impact mental well-being, especially as we navigate through the health crisis caused by COVID-19.
To learn more about Mental Health Month, please visit:
- https://www.mhanational.org/mental-health-month
- https://www.nami.org/Get-Involved/Awareness-Events/Mental-Health-Awareness-Month
In the spirit of encouraging mental well-being, BCBSRI encourages our PCP community to regularly screen for depression and substance use disorders.
BCBSRI supports and encourages use of the PHQ-9 for depression screening in primary care settings.
Why screen for depression in primary care?
- The USPS Task Force has issued guidelines for universal depression screenings and stated that 100% of patients should be screened annually for depression.
- Depression is one of the most common chronic conditions across the population. NAMI estimates that one in four adults at any given point in time are living with depression and that an estimated 16 million American adults had at least one major depressive episode in the past year.
- Screening all patients for depression in primary care can be very useful. Most providers can easily identify their patients with severe depression. However, those with mild or moderate depression often go undetected. If mild or moderate depression is identified and discussed during a primary care appointment, it can be a relief to the patient to be able to discuss their feelings openly with the PCP and be given treatment options. It can also help the patient create an action plan that may help them avoid more severe depression, and the need for more intensive medical care, in the future.
What do I do if my patient screens positive for depression?
As a PCP, you have a relationship with the patient and the opportunity to identify depression and facilitate relief. Work together with your patients to create a comprehensive treatment plan using shared decision making. Some examples of interventions may include providing patients with resources regarding depression and/or depression and chronic disease or providing them with resources regarding medication, if applicable. You may also consider offering problem solving treatment or brief supportive counseling services within your practice.
Provide patients with referrals for specialty care as needed. Not everyone with depression needs a referral for therapy. Some patients could benefit from brief interventions that could be done by a nurse case manager or other clinical staff already working in your practice. Consider options for providing supportive counseling to patients as needed, particularly as a patient is starting on a new antidepressant. It is important to stay in contact with the patient as they are managing their depression and/or other chronic conditions. Frequent check-ins with patients to provide support and education as needed will help them stay on track with managing their depression. Behavioral health case management, provided directly through BCBSRI’s behavioral health department, is also available to you as a resource for your patients. Please see below for additional information on our program and other ways to connect your patients to behavioral health resources.
BCBSRI promotes integrated behavioral health in primary care settings
The Centers for Medicare and Medicaid Services (CMS) established a code set to cover the Collaborative Care Model as well as integrated behavioral health services in primary care. In the final rules, CMS put forth specific requirements that must be met in order to submit for payment using these codes. The requirements are aligned with the foundational elements of the Collaborative Care Model put forward by CMS. To ensure adherence to these requirements, PCPs must be able to demonstrate that they are providing services under the collaborative care model or in an integrated care setting by submitting a detailed program description to BCBSRI. After BCBSRI reviews and approves the program description, the provider will be reimbursed for services provided to BCBSRI members. Please refer to BCBSRI’s Behavioral Health Integration Services including the Collaborative Care Model policy.
BCBSRI will inform the provider via email notification if their program description meets requirements. Providers will be able to submit claims 60 days after program approval. No retroactive payments will be made for services rendered. All program descriptions can be sent to Behavioralhealth@bcbsri.org.
How do I connect a patient to behavioral health services?
The behavioral health system can be confusing and overwhelming for your patients to navigate. As BCBSRI continues to expand our continuum of services for behavioral health, we realize that providers may have questions regarding the types of services available for their patients. There are several ways to learn more about behavioral health benefits and services:
- The Provider Call Center can answer questions regarding a member’s benefits, including member liability for services. They can also assist if you’re simply looking for a participating behavioral health provider. You can contact the Provider Call Center at (401) 274-4848. You can also use the Find a Doctor tool on bcbsri.com if you are simply looking for a behavioral health provider.
- The BCBSRI BH Clinical Referral Line is answered by clinical behavioral health staff. The clinical referral line can assist you in identifying a behavioral health provider, as well as providing support and guidance. The clinical referral line should not be used if there is concern of imminent danger but can be a first point of contact in non-emergency situations. The clinician, who may be a registered nurse, independently licensed social worker, or a mental health counselor, will ask questions to get a better understanding of your patient’s needs. The clinician will provide you with information about services that are available and will offer the names and contact information for providers who offer these services. You can contact the Clinical Referral Line at 1-800-274-2958. You may also share this number with your patients if they prefer to contact BCBSRI themselves.
- The BCBSRI BH Case Management Program can assist your patients in effectively managing their behavioral health conditions. Independently licensed behavioral health clinicians will work with your patients to:
- Help them understand barriers that prevent them from getting the most from their treatment or in obtaining recommended treatment.
- Help them find and obtain services or resources needed to better manage their behavioral health condition.
- Provide education and supports to help them better manage their condition.
- Coordinate care with providers to ensure you and your patient have the necessary information to provide them with the best care and support.
- Work with them to ensure they know the medications they should be taking and understand the instructions you’ve provided to them.
To refer a patient to the BCBSRI BH Case Management Program, please call 1-800-274-2958, option 2.
You may also use our automated referral form at bcbsri.com by following these easy steps:
1. Log in to the provider portal of bcbsri.com.
2. Click on Tools and Resources.
3. Click on Forms.
4. Click on Case Management Request.
5. Complete the required fields and click Go!
If your office is looking for more information regarding depression screening and follow up, please contact Jessica Walsh at (401) 459-2673 or jessica.walsh@bcbsri.org.
Another resource available to our pediatric primary care providers is the Pediatric Psychiatry Resource Network (PediPRN). PediPRN is an innovative model of telephonic consultation and collaboration between pediatric primary care and child psychiatry providers. PediPRN uses a telephonic integrated care model to improve access to quality behavioral health expertise. The service is free and provides all Rhode Island pediatric PCPs assistance with the mental healthcare needs of their patients. Pediatric PCPs can call PediPRN with a diagnostic or therapeutic question. PediPRN psychiatrists will return the call within 30 minutes. The team will assist in developing a care plan for children with various psychiatric diagnoses and complex clinical presentations. The care plan could include recommendations for psychopharmacology, therapeutic treatment, and supportive services in the community. The team will also sponsor educational opportunities via email and CME programs on pediatric psychiatry topics pertinent for the pediatric primary care community. PediPRN services are available weekdays from 8:30 a.m. to 5 p.m., except for holidays. PediPRN is offered at three Lifespan affiliates: Bradley Hospital, Rhode Island Hospital, and Newport Hospital.
Any child or adolescent in Rhode Island is eligible for this free service, however PCPs must be registered for PediPRN in advance of use. PediPRN is designed to improve access to high quality pediatric behavioral health services. For more information, please visit https://www.lifespan.org/centers-services/pediatric-psychiatry-resource-network-pediprn or contact PediPRN directly at (401) 432-1543 (1KID) or PediPRN@lifespan.org.
Behavioral health solutions at BCBSRI
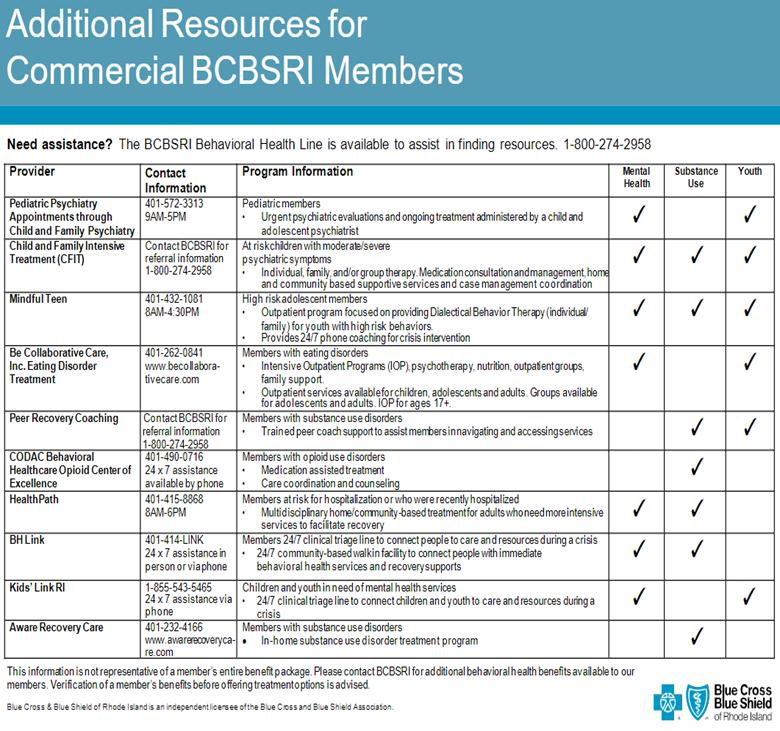
In addition to offering traditional levels of behavioral healthcare, such as inpatient, outpatient, and professional services, BCBSRI, in collaboration with community-based partners, has created a suite of behavioral health solutions for our complex members. The chart below provides an overview of some of our innovative offerings, the populations these programs serve, and which BCBSRI members can access these services.