Helpful reminders about prior authorizations in the BCBSRI MHK provider portal
One of BCBSRI’s top priorities is to give our providers the tools and knowledge necessary to submit their prior authorization requests with ease and confidence. When submitting a prior authorization request through our provider portal, remembering a few key points can eliminate data entry mistakes and ensure the process goes smoothly. Not following these points can result in a delay in processing and/or the authorization being cancelled.
Provider network status
While demographic information is important, your “provider network status" takes priority when processing prior authorization requests and drives many of the processing decisions we make with your authorization. Therefore, it is always important to ensure that if you are submitting a request for a “Par" provider your authorization represents that correctly. There are a few places in the MHK provider portal to indicate this:
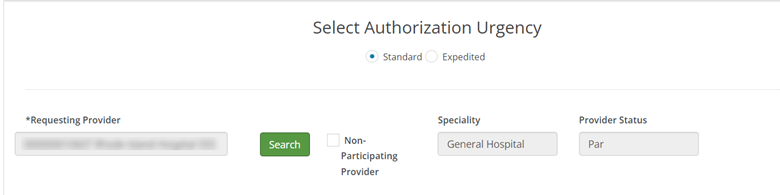
1. Requesting Provider – Provider Status: When searching for and selecting your Requesting Provider, the Provider Status box will populate indicating your provider’s network status. The “Non-Participating Provider" checkbox should never be selected unless your provider is out-of-network will BCBSRI. Only providers who are non-participating and do not have a contract with BCBSRI should select this. Most practices with access to our portal do not fall into this category. Do not check this box for any other reason even if your provider does not appear when searching.
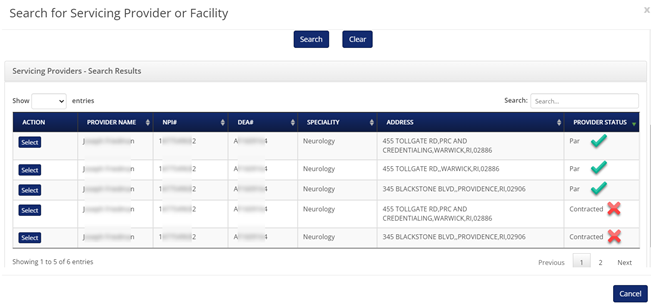
2. When searching for a Servicing Provider or Facility always select the “Par" status when available. If you do not see the desired address, please check if there is a page 2 available. While demographic information is important, provider network status takes priority when processing our authorizations.
Inpatient authorizations – Actual admit date
When submitting an inpatient prior authorization request, please indicate the “Actual Admit Date" if known. This will help save time and allows our clinicians to know exactly for which dates the prior authorization is being requested.
Behavioral health (BH) request types and Prospect members
Please only use the “BH Outpatient" and “BH Inpatient" request types for behavioral health Requests. Prior authorization requests for non-BH services using this request type will be cancelled. Please remember, we only review Prospect members for behavioral health services.
Training sessions available
Our provider relations team is hosting training sessions several times throughout the year. These sessions will be catered to the unique needs of providers, which includes prior authorization workflow, account issues, portal walk-throughs, and prior authorizations issues unique to your practice. By sharing your screen with us via Microsoft Teams, we are also able to walk you through submitting your own authorizations in real time. Please note computer access is recommended to get the full benefit of this training. Please reach out to ProviderRelations@bcbsri.org for more details.

