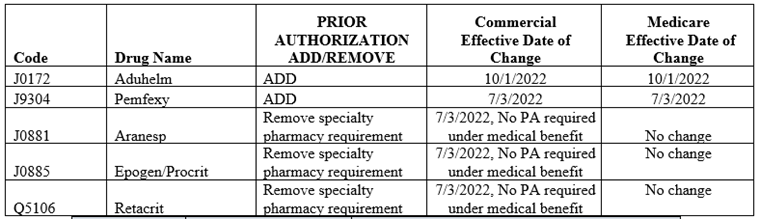
As part of our ongoing efforts to make high-quality and affordable healthcare available to our members, BCBSRI regularly reviews the list of prescription drugs we cover under our medical benefit. Our goal is to make sure that our members continue to have access to effective medications at the lowest possible cost. As a result, the following changes are being made to the Medical Drug Review (MDR) program. Existing and new prior authorization reviews will continue to be handled by our pharmacy benefits manager, Prime Therapeutics.
The prior Aduhelm policy will be archived. Please refer to the medical policy for details.
Please note removal of Specialty pharmacy requirement allows for providers to buy and bill.